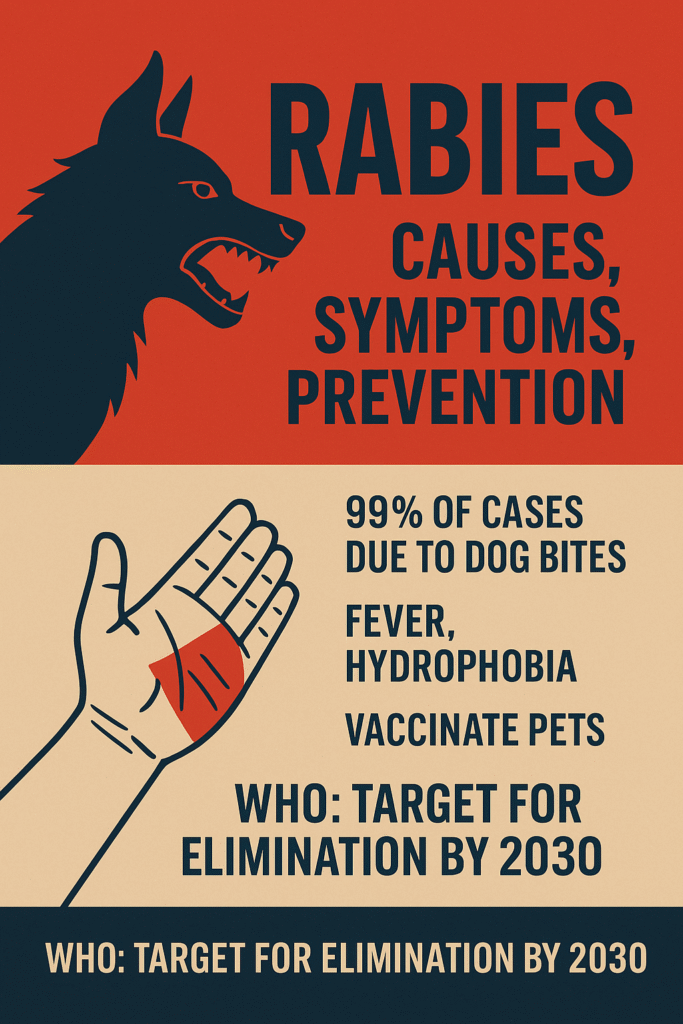
Imagine a tiny virus lurking in the saliva of an animal bite. You may not feel anything at first, yet in weeks or months, it can reach your brain and become fatal. This is rabies, a disease as old as recorded history. Despite being entirely preventable, it still kills nearly 59,000 people every year, mostly children in Africa and Asia.
Have you ever wondered why a dog bite can be more dangerous than it seems? Or why we must vaccinate pets regularly? Today, we will take a complete journey through rabies—its causes, stages, symptoms, treatment, prevention, and WHO’s mission to eliminate it by 2030.
What Causes Rabies and How It Spreads
Rabies is caused by the rabies lyssavirus, which attacks the nervous system. The virus travels silently from the bite site to the brain, making early prevention crucial.
Common Ways Rabies Spreads:
- Bites from infected animals (dogs cause 99% of human cases)
- Scratches
- Saliva contact with open wounds or mucous membranes (eyes, mouth, nose)
Primary Sources of Rabies:
- Dogs (most common in India)
- Bats (common in Americas)
- Wild animals like foxes, raccoons, and skunks
Note: Human-to-human transmission is extremely rare, with only a few documented cases through organ transplants.
Stages of Rabies Infection
Rabies progresses in distinct stages, each more severe than the last:
1. Incubation Period (1–3 months): The virus travels silently to the brain. No symptoms appear yet.
2. Prodromal Stage (2–10 days): Early signs resemble flu—fever, headache, weakness, tingling at the bite site.
3. Neurological Stage:
- Furious Rabies: Agitation, hallucinations, fear of water (hydrophobia) and air (aerophobia).
- Paralytic Rabies: Muscle weakness and paralysis; symptoms are slower and often misdiagnosed.
4. Coma and Death: Without immediate treatment, rabies is almost always fatal once symptoms appear.
Types of Rabies and WHO Bite Categories
Clinical Types:
- Furious Rabies: Most common; includes aggression and hallucinations.
- Paralytic Rabies: Gradual paralysis; less obvious but deadly.
WHO Bite Exposure Categories:
- Category I: Touching or feeding animals, licks on intact skin → No treatment needed
- Category II: Minor scratches without bleeding → Rabies vaccine required
- Category III: Severe bites, bleeding wounds, saliva contact with mucous membranes, bat bites → Vaccine + Rabies Immunoglobulin (RIG)
Recognizing Rabies Symptoms
Early Symptoms:
- Fever
- Headache
- Fatigue
- Tingling or burning at the bite site
Advanced Symptoms:
- Agitation and hallucinations
- Muscle spasms
- Difficulty swallowing
- Hydrophobia and aerophobia
- Paralysis leading to coma
Imagine a child bitten by a stray dog in rural Uttar Pradesh—the early signs can easily be mistaken for fever, but immediate medical attention can save their life.
Diagnosis: Don’t Wait for Lab Results
Rabies can be confirmed through:
- RT-PCR (saliva or spinal fluid)
- Skin biopsy (neck region)
- Blood/CSF antibody tests
- Brain tissue exam (post-mortem)
Doctors rarely wait for lab confirmation—treatment is based on exposure history, because time is critical.
Immediate First Aid After a Bite
If bitten or scratched by a suspected rabid animal:
- Wash the wound with soap and running water for 15 minutes
- Apply antiseptic like povidone-iodine or alcohol
- Avoid stitching, burning, or applying irritants
- Seek urgent medical care for vaccines and possible RIG
Tip: Quick action here can mean the difference between life and death.
Treatment: Vaccines and Immunoglobulin
Post-Exposure Prophylaxis (PEP):
- Thorough wound cleaning
- Rabies vaccine according to WHO schedule
- Rabies Immunoglobulin (RIG) for severe Category III exposures
Pre-Exposure Prophylaxis (PrEP): For vets, animal handlers, travelers:
- Two vaccine doses (Day 0 and Day 7)
- Provides baseline protection and simplifies PEP if bitten later
Proven Rabies Prevention Strategies
- Mass Dog Vaccination: Immunize at least 70% of dogs to dramatically cut human rabies cases.
- Responsible Pet Care: Regular vaccinations and check-ups, avoid stray roaming.
- Community Education: Teach children to avoid stray animals and report bites immediately.
- Universal Access to PEP: Ensure vaccines and RIG are available in rural health centers.
- One Health Approach: Collaboration across human, animal, and environmental health systems.
Nutrition and Recovery Support
While diet cannot cure rabies, it aids recovery post-exposure:
- Protein-rich foods for tissue healing
- Fruits and vegetables for immunity
- Adequate hydration
- Avoid alcohol and smoking
Who Is at Higher Risk?
- Children under 15 years
- Rural residents in rabies-endemic areas
- Animal handlers, vets, lab staff
- Travelers to rabies-prevalent countries
Global Burden and WHO’s “Zero by 30” Plan
Rabies claims 59,000 lives annually, causing significant economic loss from healthcare and livestock deaths.
The “Zero by 30” strategy, led by WHO, FAO, WOAH, and GARC, aims to:
- Eliminate human deaths from dog-mediated rabies by 2030
- Prioritize dog vaccination, vaccine access, and awareness campaigns
With community participation and timely vaccination, this goal is achievable.
Key Takeaways
- Rabies is preventable but nearly always fatal once symptoms appear
- Immediate wound washing and PEP can save lives
- RIG is essential for severe bites
- Dog vaccination and public awareness are the strongest long-term strategies
- WHO’s Zero by 30 goal can end human rabies deaths with global commitment
Frequently Asked Questions (FAQs)
1. Can humans survive rabies without treatment?
No. Once symptoms appear, rabies is almost always fatal. Immediate PEP is crucial.
2. How soon should I get the rabies vaccine after a bite?
Ideally the same day. Delay increases the risk of death.
3. Do I always need rabies immunoglobulin (RIG)?
Only for Category III exposures (severe bites or bat bites). Category II exposures require only the vaccine.
4. Is rabies contagious between people?
Extremely rare. Documented cases only occurred through organ transplants, not casual contact.
5. Can dog vaccination really eliminate rabies?
Yes. Vaccinating 70% of dogs in a community stops transmission to humans. This is central to WHO’s Zero by 30 plan.
Conclusion: Protect Yourself and Your Community
Rabies may seem like an invisible threat, but knowledge, prevention, and swift action can save lives. Wash wounds, vaccinate pets, and educate your community. Every child and adult in India deserves a future free from rabies.
Remember: The future is safe, and so can your community be.
We value your feedback! Please share your thoughts or suggestions—it helps us improve and serve you better. Your voice truly matters.
Sources –
https://www.who.int/health-topics/rabies
https://www.who.int/news-room/fact-sheets/detail/rabies
Read our article on tetanus –https://newsarmour.com/tetanus-lockjaw-causes-symptoms-prevention-global-impact/ –